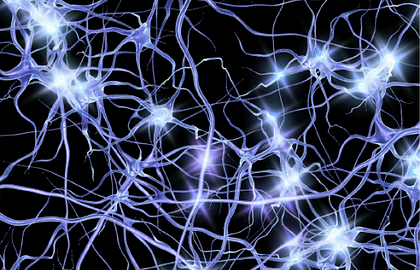
Nerve pain is pain that is caused by damage or disease that affects the nerves, spinal cord, or the brain. Your doctor may refer to nerve pain as neuropathic pain (1),(2).
When nerves are injured or damaged, they can “misfire” and send spontaneous messages to the spinal cord and brain. The spinal cord and the brain then interpret these messages as pain.
Nerve pain is often chronic, which means it can go on for several months or more with no apparent cause (3).
Nerve pain can also be caused by a number of factors including (3):

Alcohol abuse
Stroke
Spinal cord injury
Nutritional/Metabolic disorders
Infective/Autoimmune Disorders
Certain medications
The likelihood of experiencing nerve pain typically rises with age and severity of the underlying condition (3)

HOW COMMON IS NERVE PAIN?
It’s important to remember that if you suffer from pain you are not alone (3).
Nerve pain affects many people and symptoms can differ from person to person.
If you have pain that won’t go away, make an appointment to talk to your doctor.

It is estimated that
5-20%
of general
population suffer from
nerve pain. (4-9)
Nerve pain is often described as feeling tingling, pins and needles, burning, freezing, stabbing, shooting, or electric shocks (3). This pain can be constant, or may come and go, and often gets worse at night (10).

Electric shocks

Shooting/ stabbing

Burning/ On fire

Tingling/ pins & needles

Freezing
Painful areas may become abnormally sensitive if you have nerve pain. For example, sensations that would usually not cause pain, such as clothes brushing against your skin or a cold draught of air, can be intensely painful experiences (3).
DON'T IGNORE YOUR PAIN
Nerve pain can negatively impact your quality of life (12). In addition to pain, a delay in treatment or misdiagnosis of your nerve pain may lead to the development of other conditions including (12):

Anxiety
Sleep disorders
Depression
There are specific treatments available for nerve pain. If you think you have nerve pain, make an appointment to see your doctor. If you have pain that won’t go away, it’s important to get help.

HOW DOES NERVE PAIN DIFFER FROM OTHER PAIN?
Nerve pain differs from other types of pain because it directly affects the nervous system (9).
Usually, pain is the way our nervous system tells us that there is damage to a part of our body. This is called “nociceptive” pain. Unlike nociceptive pain, nerve pain arises as a result of disease or damage to the nerve itself. Nerve pain is also referred to as “neuropathic” pain. Both nociceptive and neuropathic pain can be present at the same time, which is known as mixed pain (9).
People with nerve pain may experience symptoms of stabbing, shooting or electric shocks (3). These are signs of nerve damage and are unlikely to occur with other types of pain (9).
KNOW SOMEONE WITH NERVE PAIN?
Perhaps you know someone with symptoms that sound like low back pain with a nerve pain component? If so, there are practical steps you can take to help someone experiencing ongoing pain.

References
- Health Direct Australia. Nerve Pain. 2016. Available at: https://www.healthdirect.gov.au/nerve-pain. Accessed on 1st Mar 2017.
- International Association for the Study of Pain. IASP Taxonomy. Available at: http://www.iasp-pain.org/Taxonomy. Accessed on 11th Jul 2016.
- Freynhagen R, et al. Diagnosis and Management of Neuropathic Pain. BMJ. 2009;339:b3002.
- Bouhassira D, et al. Prevalence of Chronic Pain with Neuropathic Characteristics in the General Population. Pain. 2008;136(3):380-387.
- De Moraes Vieira EB, et al. Prevalence, Characteristics, and Factors Associated with Chronic Pain with and without Neuropathic Characteristics in São Luis, Brazil. J Pain Symptom Manage. 2012;44(2):239-251.
- Elzahaf RA, et al. Translation and Linguistic Validation of the Self Completed Leeds Assessment of Neuropathic Symptoms and Signs (S-LANSS) Scale for use in a Libyan Population. Pain Pract. 2013;13(3):198-205.
- Ohayon MM, et al. Prevalence and Comorbidity of Chronic Pain in the German General Population. J Psychiatr Res. 2012;46(4):444-450.
- Torrance N, et al. The Epidemiology of Chronic Pain of Predominantly Neuropathic Origin. Results from a General Population Survey. J Pain. 2006;7(4):281-289.
- Toth C, et al. The Prevalence and Impact of Chronic Pain with Neuropathic Pain Symptoms in the General Population. Pain Med. 2009;10(5):918-929.
- Meyer HP. Neuropathic Pain - Current Concepts. SA Fam Pract. 2008;50(3):40-49
- Pop-Busui R, et al. Diabetic Neuropathy: A Position Statement by the American Diabete Association. Diabetes Care. 2017;40(1):136-154.
- Harden N, et al. Unmet Needs in the Management of Neuropathic Pain. J Pain Symptom Manage. 2003;25(5 Suppl):S12-17.
- Haanpää ML, et al. Assessment of Neuropathic Pain in Primary Care. Am J Med. 2009; 122(10Suppl):S13-21.



 HOME
HOME

