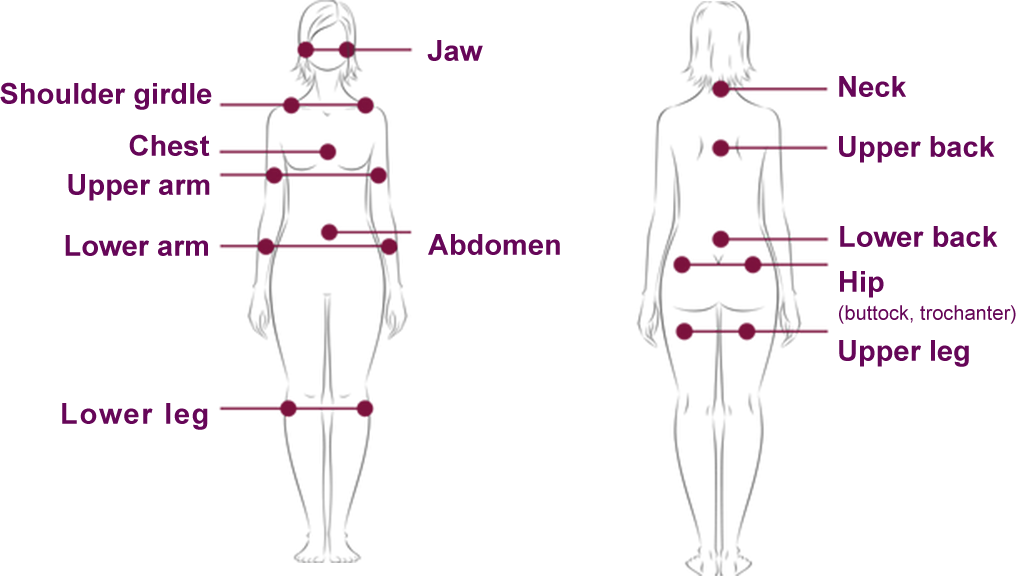
Fibromyalgia is a chronic condition (lasting more than 3 months) that is characterized by widespread muscle pain on a number of areas of the body (1),(2):
Fibromyalgia is often accompanied by other symptoms such as fatigue, sleep disturbances and difficulties in remembering (2),(3).
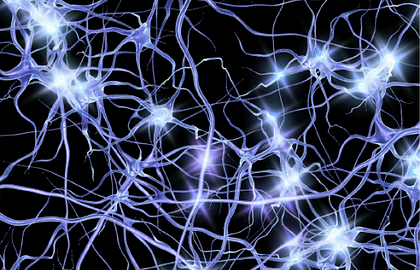
Although the causes of fibromyalgia are not fully understood, many researchers believe “central sensitization” is involved.(3) This means the central nervous system (brain and spinal cord), may have a stronger response to a stimulus, such as touch (2).
Factors or conditions that may trigger the development of fibromyalgia include (2):
Family history of
chronic pain
Some infections , E.G.
VIRAL HEPATITIS
Rheumatoid arthritis
Psychological
stress
Physical / Emotional
trauma
Lupus
If you are experiencing widespread muscular pain, it's important to talk to your doctor to describe your symptoms.
HOW COMMON IS FIBROMYALGIA?
Fibromyalgia is difficult to diagnose and is often missed. The first step towards getting the right help and treatment is a correct diagnosis.
Make sure you describe your symptoms to your doctor to help them diagnose your pain.
Fibromyalgia affects an estimated 2.7% of the population, or 200 million people worldwide (4).
Women are 3x more likely to develop fibromyalgia than men (4).
Fibromyalgia is a condition that is characterized by chronic widespread pain (3). It is often accompanied by other symptoms such as fatigue, memory problems, and sleep and mood disturbances (2).
The widespread pain in fibromyalgia has been described as aching, throbbing, shooting, stabbing, or burning (5).

Aching

Throbbing

Shooting

Stabbing

Burning
People with fibromyalgia frequently experience a myriad of other conditions, such as arthritis, migraines, depression and anxiety, and insomnia (6).
MEDICAL CONDITIONS
Nearly 9 in 10 have chronic
joint pain or arthritis
Almost two-thirds suffer from
migraines or chronic headaches

Over 50% have high
cholesterol
Around half are obese
(BMI ›30)
More than 2 in 5 have
high blood pressure
Nearly one-third have
irritable bowel syndrome
MENTAL HEALTH CONDITIONS

Around 3 in 4 suffer
from depression

Over half experience
anxiety
SLEEP CONDITIONS

ABOUT 1 in 2 suffer
from insomnia

ALMOST one fifth have
restless leg syndrome
It is important to describe the pain you are experiencing to your doctor as it may assist in helping make the right diagnosis and identifying the most appropriate treatment options.
DON’T IGNORE YOUR PAIN
Fibromyalgia can largely affect your quality of life (5).
In addition to pain, a delay in treatment or misdiagnosis of your fibromyalgia may further add to the burden of management of other existing co-morbidities like (6):

Arthritis
Obesity
High blood pressure
Migraines

Anxiety
Depression
Insomnia
Type 2 diabetes
Irritable bowel Syndrome
If you think you have fibromyalgia, make an appointment to see your doctor.
If you have pain that won’t go away, it’s important to get help.

Fibromyalgia pain differs from other types of pain as it can be felt in a number of areas of the body (1),(2). The pain experienced occurs frequently, at a high intensity, and in deeper tissues such as the muscles (3),(7).
In contrast to nerve pain syndromes, nerve injury is not apparent in the majority of people with fibromyalgia (7).
Fibromyalgia may affect different people in different ways. It is important to describe your symptoms to your doctor.
KNOW SOMEONE WITH FIBROMYALGIA?
Perhaps you know someone with symptoms that sound like fibromyalgia? If so, there are practical steps you can take to help someone experiencing ongoing pain.

References
- Arnold LM, et al. Efficacy and Safety of Pregabalin in Patients with Fibromyalgia and Comorbid Depression Taking Concurrent Antidepressant Medication: A Randomized, Placebo-Controlled Study. The Journal of Rheumatology. 2015;42(7):1237–44.
- Clauw D. Fibromyalgia and Related Conditions. Mayo Clinic Proceedings. 2015;90(5):680–92.
- Bellato E. et al. Fibromyalgia Syndrome: Etiology, Pathogenesis, Diagnosis, and Treatment. Pain Res Treat. 2012;2012:426130.
- Queiroz LP. Worldwide Epidemiology of Fibromyalgia. Current Pain and Headache Reports. 2013;17(8):356.
- Damsky D. Getting the Point About Fibromyalgia. Nursing. 2007;37(2):61–4.
- Vincent A, et al. A Cross-Sectional Assessment of the Prevalence of Multiple Chronic Conditions and Medication Use in a Sample of Community-Dwelling Adults with Fibromyalgia in Olmsted County, Minnesota. BMJ Open. 2015;5(3):e006681.
- Koroschetz J, et al. Fibromyalgia and Neuropathic Pain – Differences and Similarities. A Comparison of 3057 Patients with Diabetic Painful Neuropathy and Fibromyalgia. BMC Neurology. 2011;11:55.



 HOME
HOME

